Personalized health care is an overarching framework for proactive, personalized health care that provides individuals with a personal health plan to maximize their health and minimize disease. It utilizes predictive technologies to establish each individual’s health risks and facilitates patients’ engagement in their health along with the development of plans and a care delivery system designed to achieve the best health outcomes.
The Personalized Health Care Approach
Personalized, Predictive, Preventive, Participatory
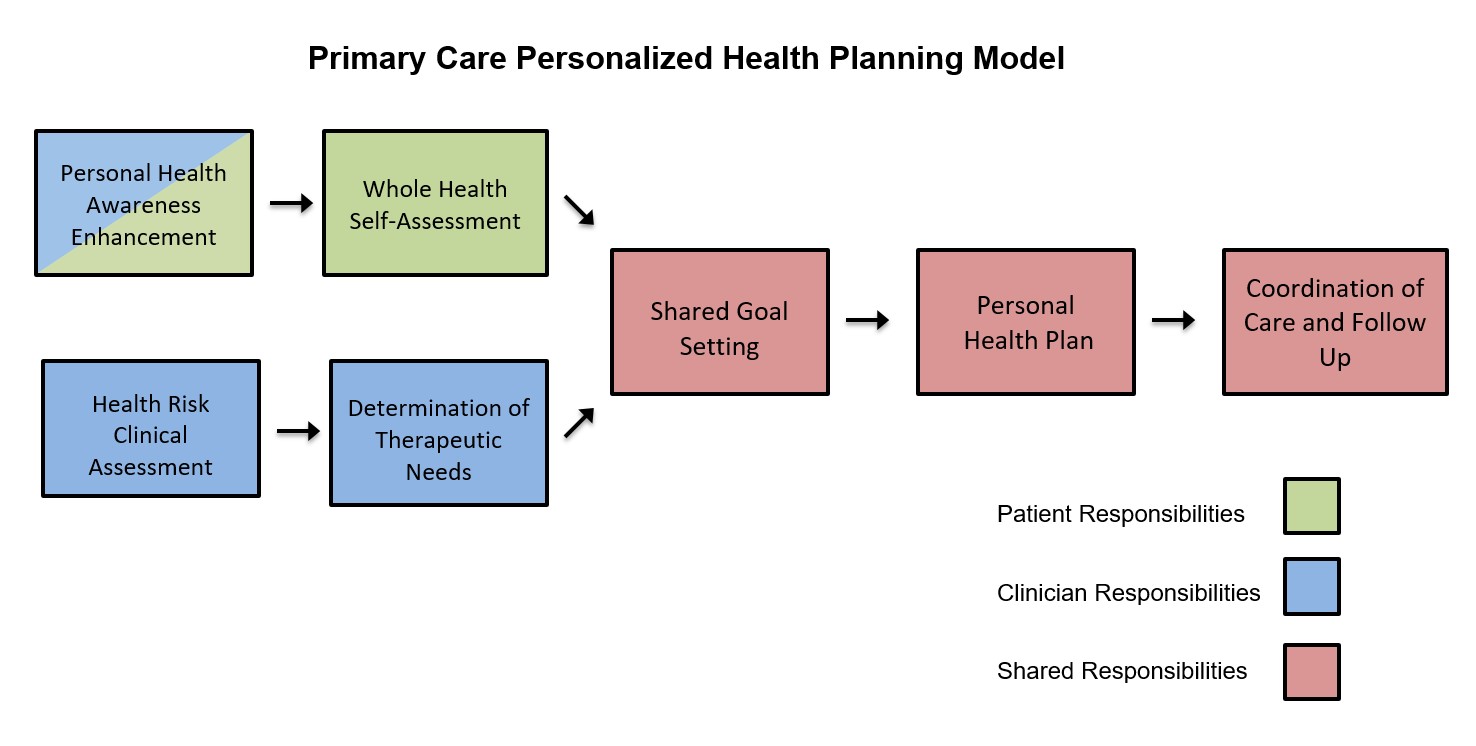
Personalized health planning is the key feature of personalized health care as it anticipates the individual’s specific health needs and develops a coordinated means to achieve them. The personal health plan is developed collaboratively by the provider and the patient and utilizes comprehensive health risk assessment as the basis for both enhancing health and well-being and mitigating and tracking disease over time. Greater collaboration between patient and provider replaces the traditional physician-dominated dialogue with more effective patient-physician partnerships and continuity of care. The patient’s needs and goals for their health, wellness, and disease mitigation drive the planning process and nature of the plan. The personalized health planning framework provides an operational care model for delivering personalized, proactive, patient-driven care to individuals with a diverse range of needs.
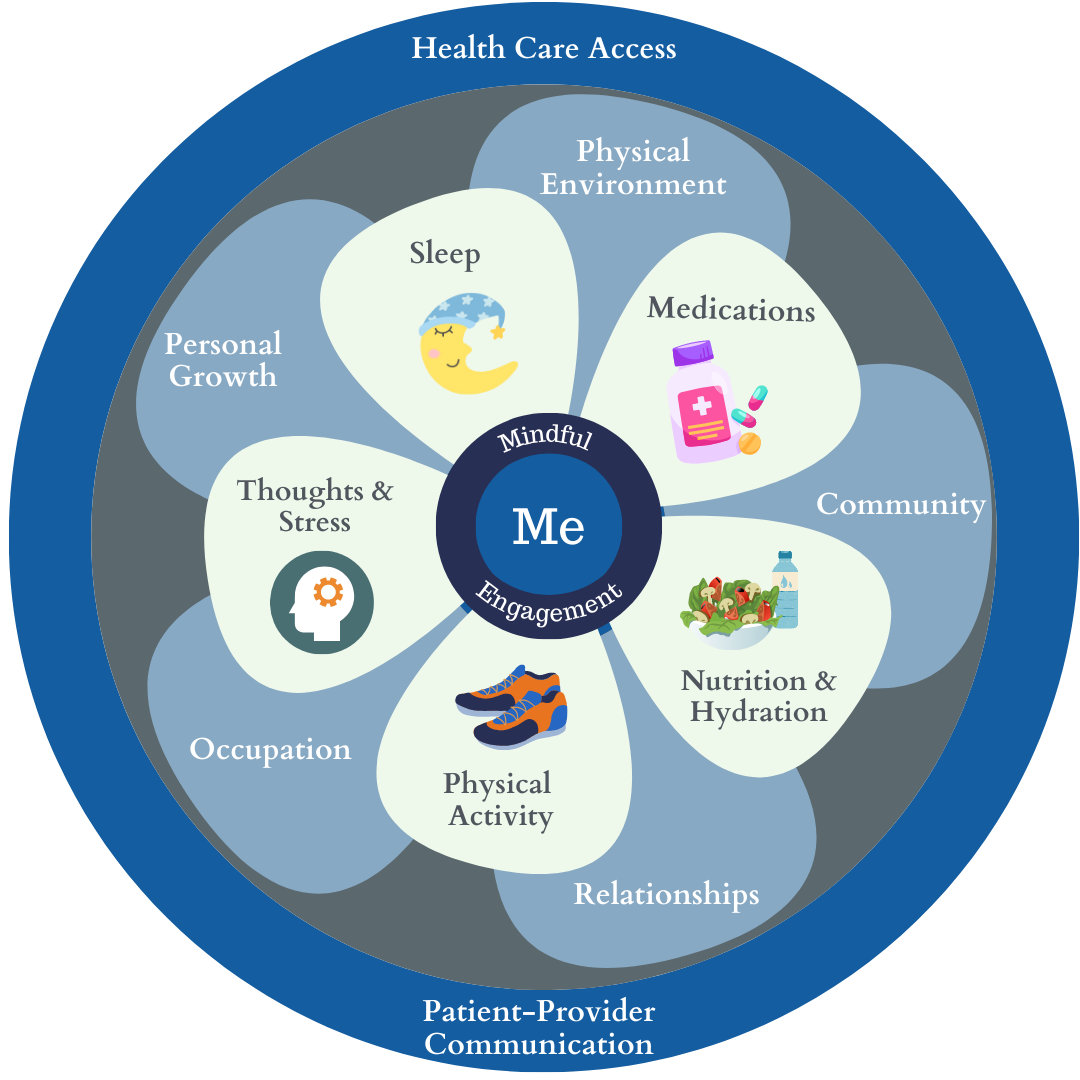
In our model, Personalized Health Planning (PHP) creates the process for engaging the patient in their care. It identifies needs and desires for their own health with therapeutic plans and support systems to achieve meaningful goals. We focus on empowering patients to adapt the behaviors that have the greatest impact on the ability to manage their chronic diseases. These include medication adherence, proper nutrition and hydration, physical activity, restful sleep, stress reduction, and mental and emotional well-being. The connection to mind-body is also encouraged through the practice of mindful meditation to be better attuned to one’s self and behaviors.
Five key steps outline the PHP process:
- The patient completes a self-assessment of health needs, preferences, and goals.
- The clinician assesses the patient’s health status and health risks using the best available conventional, genomic, and other precision diagnostic tools and identifies optimal risk-mitigation and therapeutic goals for the patient.
- The patient’s health coach meets 1:1 with the patient and uses the clinician’s health assessment and the patient’s self-assessment to establish shared goals.
- The shared goals are incorporated into the personal health plan. The clinician chooses appropriate metrics for monitoring progress.
- The clinician coordinates care with the patient’s care team and arranges for appropriate follow-up.
For more details about Personalized Health Planning, see our piece in NEJM Catalyst.
Why Is Personalized Health Care Important?
To improve the health of the individual and the nation, health care must move from its current reactive and disease-centric system to one that is proactive and focused on wellness, disease prevention, and the precise treatment of disease. With the boom in predictive and precision technologies, targeted therapies, and the growing evidence of benefits from effective patient engagement strategies, this shift is now possible. Personalized health care is designed to do this.
Personalized health care is based on the concept that each of us is born with inherited susceptibilities or resistance to various diseases. Genetic susceptibilities for most chronic diseases are greatly impacted by what we do and what we are exposed to.
Development of Disease
The natural progression of disease over time is a consequence of inherited susceptibility (genetic inheritance) and exposure to environmental factors, including lifestyle. As individuals age, depending on their genetic inheritance along with what they do and what they are exposed to, they may develop a chronic disease which progresses over time. It is becoming more widely understood that chronic disease is often the result of multiple factors rather than one single factor.
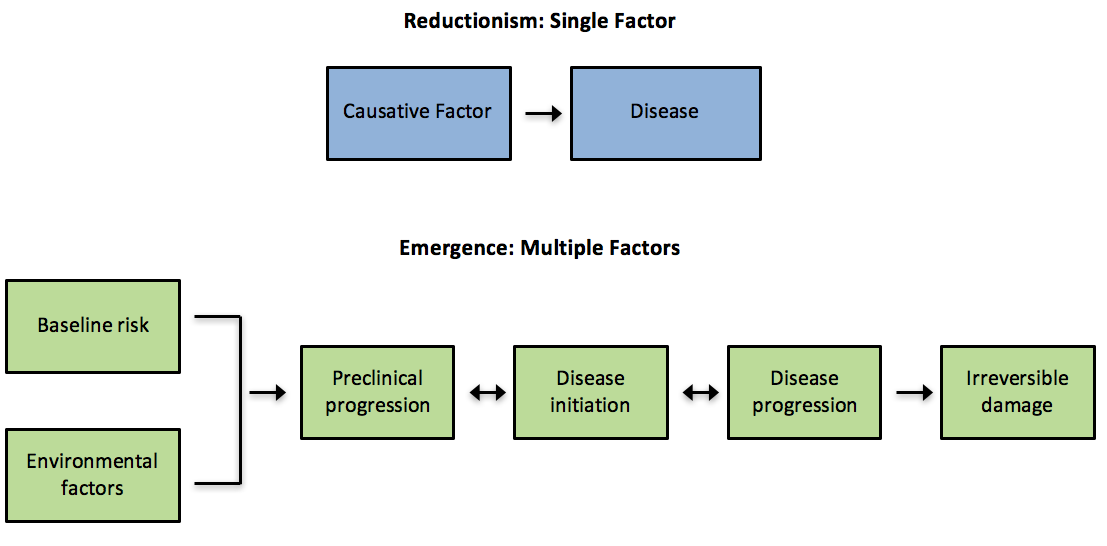
Different diseases (i.e., cardiovascular disease, metabolic disease, cancers) have different rates of development. In any case, for a long portion of its development, a disease is not clinically apparent although in many cases it could be detected with appropriate attention and diagnostics. Once signs and symptoms develop, it is generally late in the disease development process and the degree of reversibility is reduced and the cost of treatment increases.
Trajectory of Chronic Disease
The Inflection Curve of Disease demonstrates the general trajectory for the development of disease over time and where the individual and the health care system might intervene. As a chronic disease progresses, the chances of reversal of the disease decrease and the costs increase. Thus, the earlier the intervention, the better.
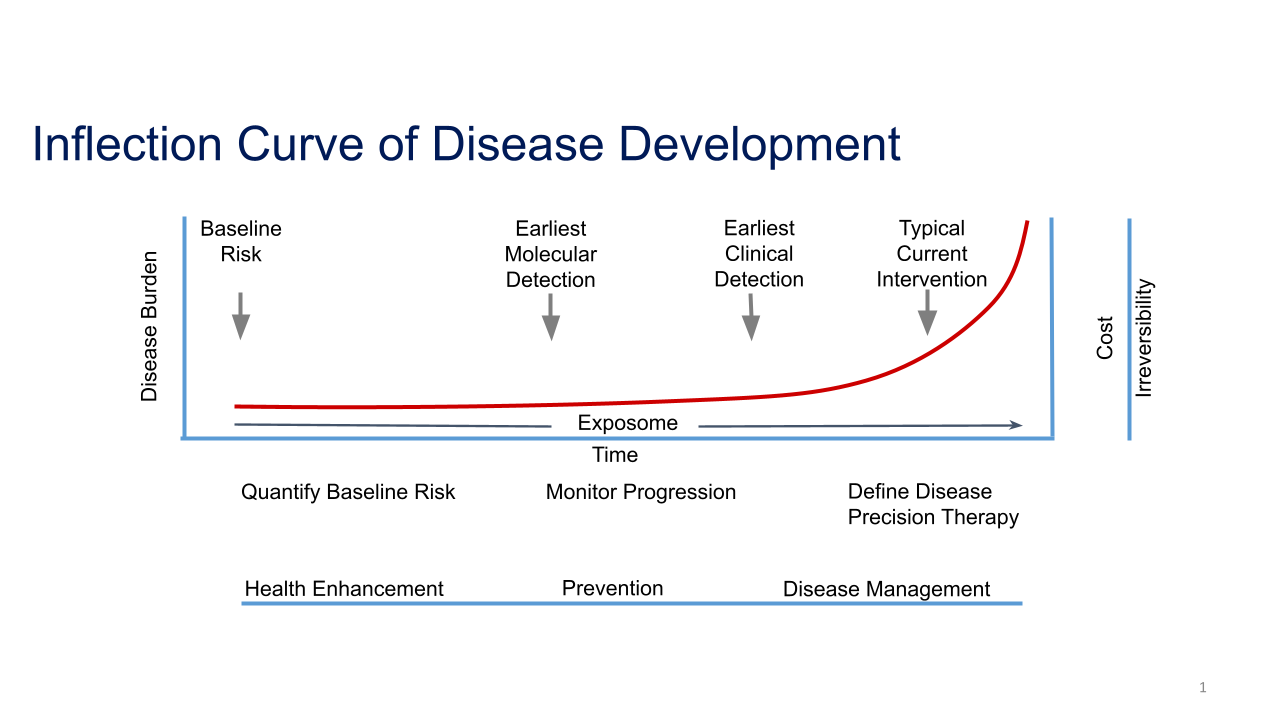
There are three time periods concerning the trajectory of chronic disease. The right portion of the curve is what we hope to avoid; it is when the burden and cost of poor health takes its toll on individuals and society. Early 21st century health care has made great strides in being able to treat disease once it occurs. Our medical technologies are far better than before, but once disease manifests, intervention is often expensive and minimally effective at reversing the underlying problem. For some people, disease development is unavoidable and personalizing therapy and disease management can substantially improve health outcomes. But for many, the burden of established chronic disease can be greatly mitigated if it is addressed proactively before it develops.
The middle of the curve is the period during which primary prevention is most important. If an individual’s health risks are known, their providers can begin working with them on what is preventable. This can be done through education about lifestyle changes for health enhancement (like healthy diet and exercise), engaging individuals in their health, continuously monitoring risk markers for disease progression, and at times, medications to minimize disease development.
Furthest to the left of the curve, before a disease begins to develop, provides the greatest opportunity for improving health. Based on an individual’s characteristics, genetics, and environment, one can begin to quantify his or her disease risks and develop a plan to prevent them. At this point, engaging the individual in lifestyle changes to minimize their disease risks can have the greatest impact. By doing so, health care can focus on shifting the interventions to the left of the curve resulting in a far more efficient and effective health care delivery model.
