Traditional Chinese Medicine and Its Clinical Potential to Fight Chronic Pain
As the burden of chronic disease continues to rise, patients and clinicians may seek additional treatment pathways to supplement conventional Western medicine. Trends toward holistic and patient-centered care models increasingly draw treatment-seekers toward non-conventional therapies with a history of use outside of Western medicine. These complementary and alternative medicines (CAM), as defined by the National Center for Complementary and Integrative Health (NCCIH), support or supplant previous treatment options:
- Complementary medicines are non-mainstream practices used in conjunction with conventional medicine
- Alternative medicine are non-mainstream practices that replace conventional medicine
CAM therapies sourced from a number of cultures include practices such a mindfulness-based interventions, yoga, and chiropractic manipulation, all of which have been largely embraced by the Western public. Similarly, Western health systems are gradually expanding
Traditional Chinese Medicine (TCM) services, namely acupuncture, tai chi, and herbal medicine. Western health systems’ reluctance to embrace TCM has been rooted in historical biases and deferred efforts to establish an evidence base for promising TCM therapies. The authority of Evidence-based medicine (EBM) has thus challenged traditional institutions like TCM to demonstrate clinical effectiveness before being fully embraced in the West. This has led to a promising and expanding field of research into exploring a diverse range of clinical applications for different TCM modalities.
One of the more notable researchers to bridge these cultural conventions, Tu Youyou, was awarded the 2015 Nobel Prize in Physiology or Medicine for her role in pioneering a new class of antimalarial drugs near the end of the Vietnam War. Tu’s team first introduced the scientific method and publication to Artemisia annua (qīnghāo青蒿), a type of wormwood known to TCM practitioners since the 4th Century as a robust treatment of malarial fever, and was lauded internationally for her proof of cross-system application for TCM. She and researchers like her have helped foster the gradual adoption of select TCM treatments by modern health systems and propelled greater scientific inquiry of its potential benefits.
Investigations into TCM’s ability to effectively manage chronic pain are of particular clinical relevance, though the exact analgesic mechanisms behind certain practices such as acupuncture remain a point of contention. Nevertheless, TCM services now occupy a rapidly growing space in holistic health assessment, preventive medicine, and disease treatment, particularly in populations experiencing chronic health outcomes. Active duty soldiers and Veteran populations have been among the most receptive to TCM interventions due to efforts to find low-risk CAM therapies to treat chronic pain. Chronic pain and subsequent opioid use as a treatment tool are significantly higher in soldiers than in the general population: 44 percent of recently returned active-duty American soldiers report chronic pain and 15.1 use some level of opioids for pain management. However, due to recent changes in opioid prescription standards, only half of these soldiers report the moderate to severe pain for which opioid prescription is now recommended. These changes reflect the heightened awareness of opioid abuse risk given the addictive nature of these medications. It is thus recommended that providers prescribe the lowest effective dose to reduce the risk of complications. In the absence of sufficient alternative therapies, some level of opioid use remains necessary for many Veterans given the higher prevalence of chronic pain in this population. When the risks outweigh the benefits of opioid therapy, it is necessary to pursue non-opioid and non-pharmacological alternatives.
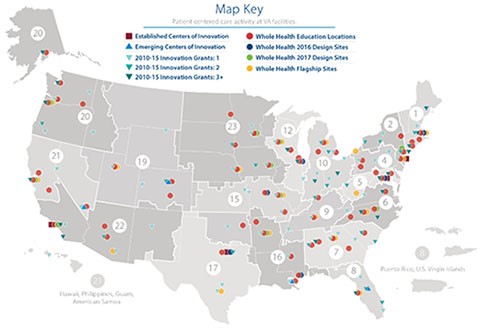
CAM therapies used as part of a holistic treatment plan, which also includes conventional medicine, may help mitigate overreliance on and potential abuse of high-dose opioid prescriptions while facilitating lower-risk pain-coping mechanisms. Acupuncture (zhāzhēn扎针) is being largely embraced by these populations as the pressing need to reduce opioid use drives the VA and Department of Defense to invest $81 million in CAM and non-drug therapies over six years. Additionally, the VA’s Whole Health System (Figure 2), which seeks to transform the VA Health System to a patient-centered care model that emphasizes wellness and prevention, has expanded the availability of complementary and integrative services. These services include traditional acupuncture for its reported success in treating chronic pain and PTSD as well as battlefield acupuncture, a modified version of the TCM practice that may offer more immediate pain relief. The expansion of these CAM offerings coincides with an intentional decrease in opioid prescription rates constituting a 50 percent change at several dozen VA facilities since 2012.
Beyond TCM’s application to opioid management, TCM’s favoring of a holistic treatment of the body over specifically targeted medicines help fill in the diagnostic and treatment gaps left by conventional medicine. This is particularly true for diagnoses of exclusion, like fibromyalgia and IBS, for which we have limited understanding of the pathophysiology at the root of these conditions. Acupuncture and other TCM practices have yielded encouraging clinical results, including that the practice of Tai Chi (tàijíquán太极拳) has myriad benefits for patients of musculoskeletal pain, depression, and chronic heart failure. Patients with such chronic conditions may find greater validation in a holistic assessment of their health needs and greater relief for symptoms after exhausting conventional medicine options. TCM may also offer clinical researchers new practice patterns for diagnosis and treatment through pattern differentiation, the TCM practitioner’s procedure for making differential diagnoses and modifying diagnoses based on responsiveness to treatment. This methodology has been incorporated into studies as a promising tool to identify a subset of patients with Rheumatoid Arthritis (RA) who will be more responsive to biomedical therapy.
As Western health systems continue to innovate ways to employ CAM therapies to provide more personalized, proactive, and patient-centered care, it is important to avoid appropriative behavior by not laying claim to the conception of the medical practices themselves. TCM, like other CAM therapies with non-Western origins, is an ancient institution that is uniquely organized around its home culture’s values and belief system. TCM’s growing clinical applications should instead expedite greater synthesis of global health practices in modern health systems. Western providers and patients alike may feel empowered to consider TCM practices and holistic principles as part of their comprehensive solicitation for better health outcomes.
