The Importance of Addressing Language Barriers in the US Health System
“What the Scalpel is to the Surgeon, Words are to the Clinician…. the Conversation Between Doctor and Patient Is the Heart of the Practice of Medicine.”
– Woloshin S, et al., 1995
Currently, 1 in 15 people living in the US have Low-English Proficiency (LEP) and it is predicted that this number will increase to 67 million by 2050. As detailed by the Title VI of the Civil Rights Act of 1964, federally funded health institutions must provide interpreter services for LEP patients; however, due to financial restrictions, this federal requirement is not always enforced. As a result of language barriers, LEP patients exhibit a lower return rate for follow-up visits, which can result in poorer health outcomes. As the number of LEP people living in the US increases, the need for medical interpreters and bilingual medical staff becomes more essential.
Who are Medical Interpreters?
Medical interpreters serve as mediators for LEP patients and doctors to allow for improved communication between the two parties. There are medical interpreters that work over the phone and others who work in the physical clinical settings. According to a systematic review of the literature, the presence of a medical interpreter has shown to improve patient engagement, reduce medical errors, and facilitate efficient communication.
The Value of Effective Communication with LEP Patients
The benefits associated with the use of language services in clinics and hospitals include, but are not limited to, 1) increased quality of care, 2) improved patient safety outcomes and 3) lower utilization of costly medical procedures.
1. Increased Quality of Care
Quality of care for LEP patients often is based on two factors: language and cultural values.
Language
With increased access to language services, many LEP patients are more likely to understand the significance of medical procedures and medications. A study by the University of California, San Francisco shows that there were differences between the rates of informed consent documentation of LEP and English-speaking patients. According to the article, such a discrepancy could be attributed to the lack of documentation of interpreter services during the consent process. As a result, LEP patients were less likely to contain consent forms in their charts than English-speaking patients, indicating a disparity in the implementation of informed consent for the LEP population. Another study conducted in 2007 showed that LEP patients who received no interpreter services were less likely to be aware of medical implications and were less satisfied overall about their medical care. With facilitated communication, patients will be more likely to be informed and able to make educated medical decisions.
Cultural Values
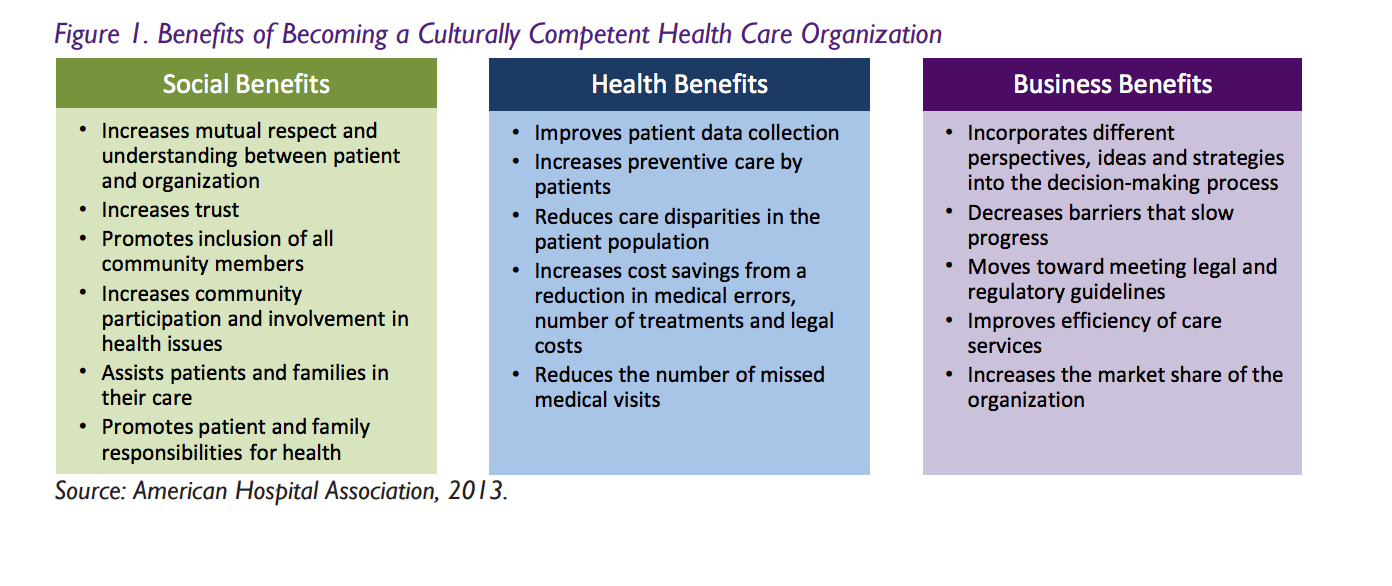
Increasing the quality of care for LEP patients also means taking into account cultural differences. Cultural values and principles may look very different for the provider and the patient. Figure 1 shows a list of the social, health and business benefits of providing culturally competent health care. By ensuring medical interpreters and providers are trained in cultural competency, the higher the likelihood that LEP patients will be able to understand and follow certain medical treatments. The National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health and Health Care were created by the Office of Minority Health in the US Department of Health and Human Services. CLAS provides a baseline for health institutions to strive for and aims to standardize the quality of care provided in health institutions. With these endeavors in mind, it is important to realize the significance of a patient’s personal values. By doing so, this allows for culturally-appropriate personalized medical care that encourages patient engagement. By implementing such cultural cooperation, the provider is able to deliver precise and preventive medical care that contains realistic outcomes for the patient.
2. Improved Patient Safety Outcomes
Patient safety can be improved for many LEP patients when there are sufficient language resources available. According to a study in 2007, 49.1% of LEP patients received some kind of physical harm as a result of a medical error. By documenting language disparities in hospital settings, the study shows that health institutions have the potential to improve LEP patient safety. In addition to this documentation, increasing awareness of language resources among medical staff and patients can help to ensure interpreter services are being utilized. Many LEP patients do not realize they have a right to request a medical interpreter and as a result fail to use these services. Therefore, having informed health providers who understand how to utilize language services can help ensure more doctors and LEP patients will be better equipped to prevent safety risks and promote effective care.
3. Lower Utilization of Costly Medical Procedures
Even though it is not financially possible to have bilingual providers and medical interpreters in every language, there are cost-effective ways to meet the demand for these language services. A study conducted by UC Berkeley shows that by improving the efficiency of video conferences, call centers and an online presence, language services can increase the span of their services so that they can reach more people with an increased use of technology. The presence of a language barrier has been shown to be associated with higher rates of costly resource utilizations for diagnostic testing and increased emergency department visit times in a pediatric emergency department. When no interpreter services are available to overcome the language barrier between the patient and the health provider, medical staff must perform precautionary health measures to identify what the patient has without any context or patient history. By introducing medical interpreter services, there is evidence of reductions in emergency department visits and a decreased utilization of extraneous medical exams.
Conclusions
”When you can’t speak to your patient in their native language, you do the best you can. No system of translation will ever be foolproof and you will never be able to duplicate that trust you establish when you speak the same language.”
– Fein, New York Times, 1997
With a growing number of LEP people in the US, what does the future hold for LEP patients in the health care system? It is well understood by many providers the significance of being able to communicate effectively with patients; however, the issue lies with resources and funding of medical institutions. In an ideal world, medical interpreters would be widely available to interpret for a large population. Patients’ cultural values would be taken into account when helping to plan out their treatment options and health providers would ensure patients are properly informed on all aspects of their condition in their native language. However, due to financial restrictions, language services are not always available despite their proven benefits. As the health care system begins to become more personalized and preventive, it is important to push for the improvement of patient communication. By doing so, medical providers will be able to empower patients with medical knowledge that enables LEP patients to make realistic decisions on their health. As language barriers persist in the US health care system, policy makers and health care leaders must prioritize efforts to enable accurate and culturally-sensitive communication to improve quality of care, fortify patient safety and lower the utilization of medical procedures.
